Wearable-monitored skin temperature can be an index of infection

This blog article outlines the findings of the study “Monitoring skin temperature at the wrist in hospitalised patients may assist in the detection of infection”, published earlier this January 6, 2020, on Internal Medicine Journal.
Measuring body temperature is one of the oldest clinical tools known to help diagnose infection. From when the time-temperature measurement was first introduced following the detailed reports of Carl Wündelich in the mid-19th century, physicians have focused on the presence or absence of fever based on a single time point measurement.
Increasing evidence, however, suggests that body temperature patterns and variability may convey other meaningful clinical information, regardless of the actual temperature, and be an earlier indicator of a potentially life-threatening condition.
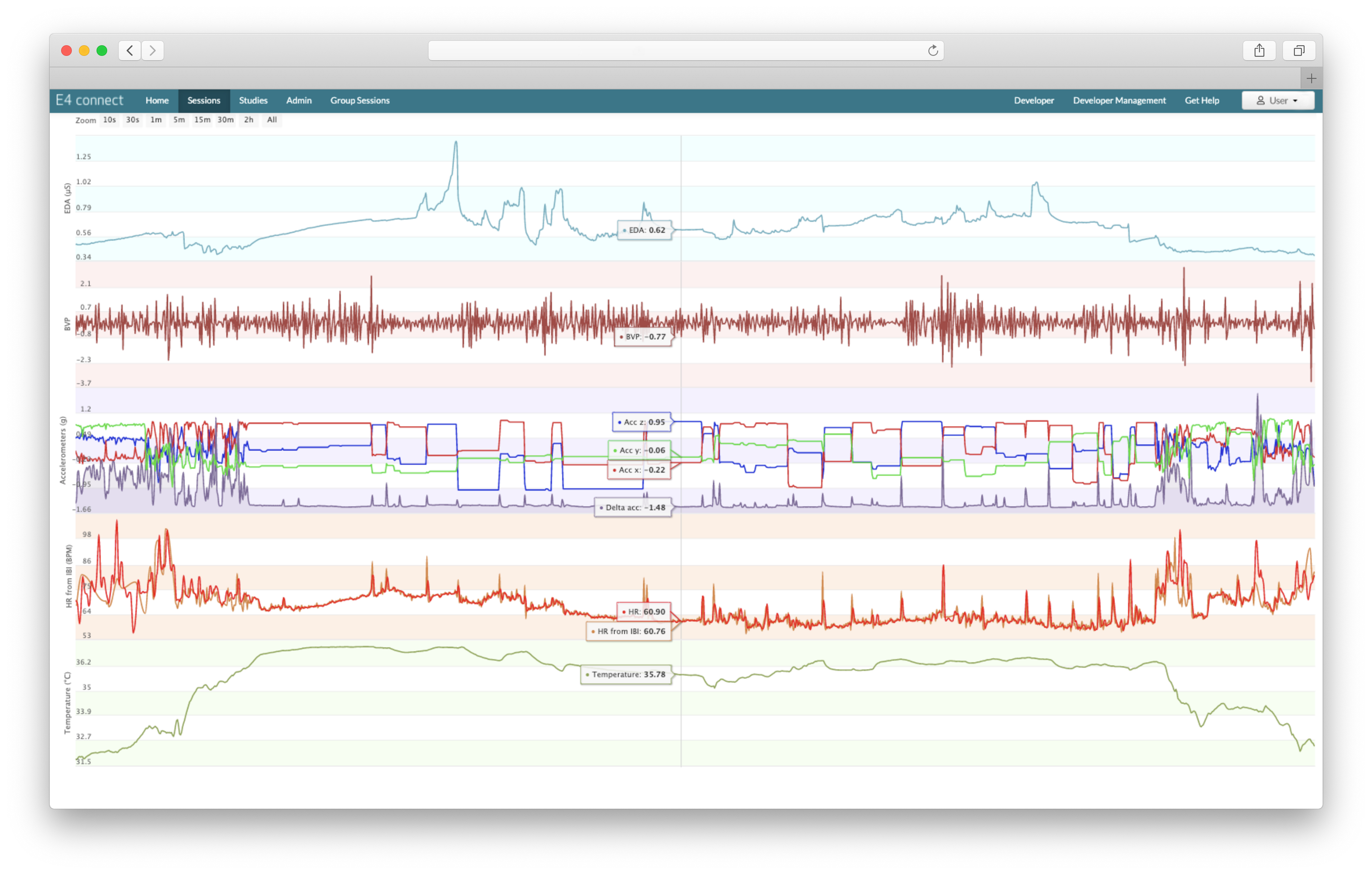
The recent advancements in wearable technology have produced wearable devices that can precisely measure skin temperature continuously and automatically. The study we are focusing on in this article assessed the feasibility of using a clinical-grade wearable device, the E4 wristband, to measure peripheral body temperature and detect infection in patients with kidney disease. The researchers also evaluated whether peripheral temperature and other physiological variables could be used as an index of infection.
How the E4 wristband was used to identify active infection
The pilot study was conducted at The Royal Melbourne Hospital on an unselected population of patients admitted to the adult nephrology ward, and included patients with chronic kidney disease (CKD), on dialysis, and with kidney transplants.
Participants wore the E4 wristband for a minimum of 4 hours, recording heart rate, heart rate variability, peripheral temperature, respiration rate, and oxygen saturation. Eighty-eight temperature data sets were available for analysis. The researchers employed simple algorithms to see if the E4-measured peripheral body temperatures could be used to classify infection. They found that a larger percentage of temperature measurements over 37C was associated with active infection.
Most of the key trials in continuous temperature monitoring have been conducted in intensive-care settings. Continuous temperature monitoring is potentially more useful in a ward setting or for patients at home as a tool for detecting infection before they develop symptomatic shock and end-organ dysfunction, requiring intensive and expensive support. The cost of sepsis management in U.S. hospitals ranks highest among all admissions: in 2013, sepsis management accounted for more than $24 billion in hospital expenses, representing 13% of total U.S. hospital costs.
The study at the Royal Melbourne Hospital appears to be the first study investigating continuous temperature monitoring in patients with renal failure in an inpatient medical ward environment.
Their findings suggest that continuous wrist monitoring may be as good as, or perhaps better than, conventional recording of intermittent oral temperatures in a ward setting.
The value of continuous vital signs monitoring
Various studies have demonstrated that the variability of other physiological variables apart from temperature (namely heart rate and respiratory rate) has the potential to assist with early detection, management, and treatment of infection.
As shown by Andrea Bravi and colleagues, the host response to infection or injury is a complex nonlinear system. Continuous monitoring over time of the system as a whole allows tracking the changes (i.e. trajectory) in the system state. Continuous vital signs monitoring and variability analysis, therefore, can add incremental value to intermittent point-in-time vital sign measurement, with the potential of detecting infection in a more timely manner.
Early identification (and consequent treatment) of infection has been proven to reduce mortality, and it has been recognized as a time-sensitive emergency. Even more so in the midst of a high-impact respiratory pandemic.
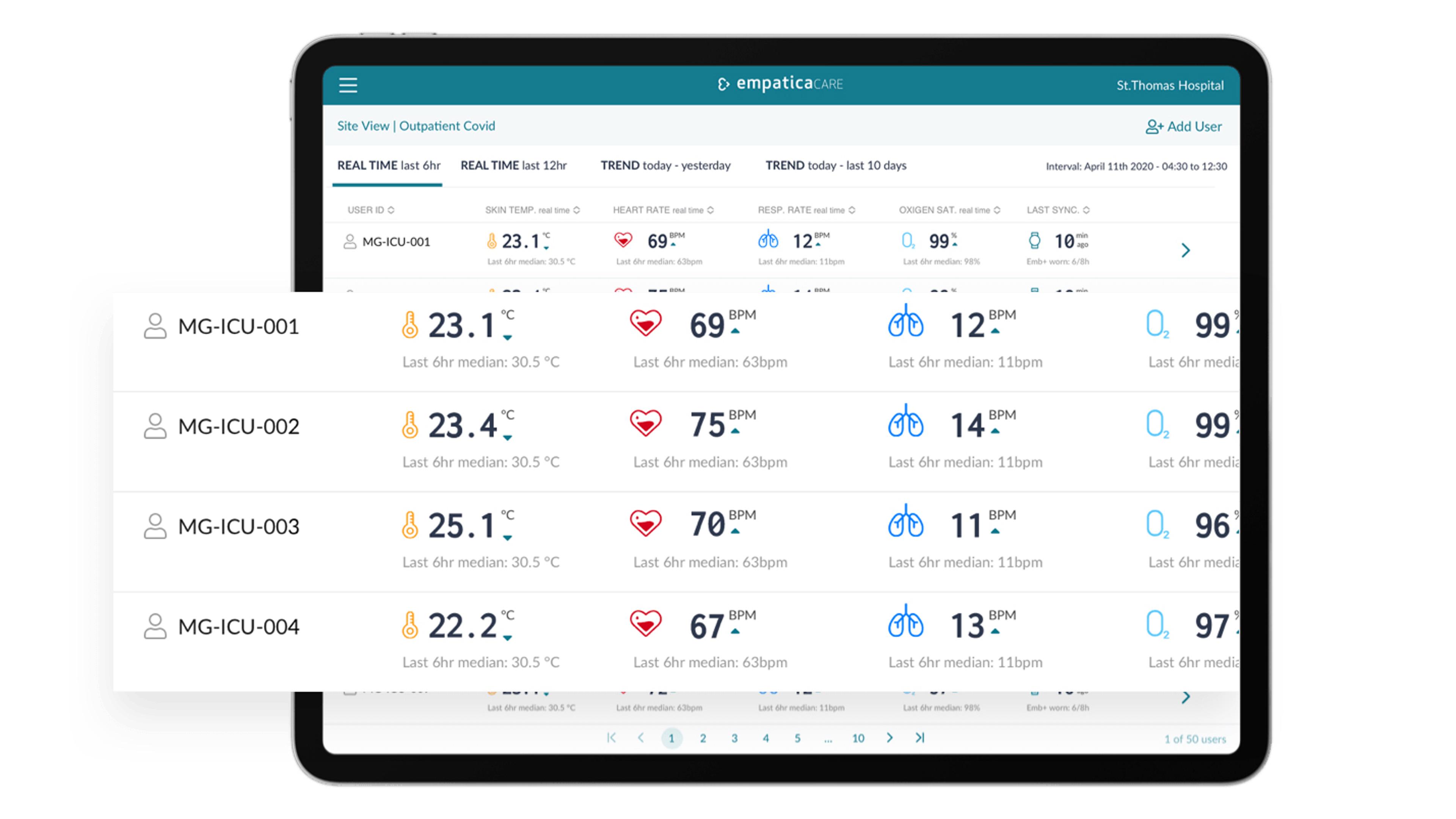
With the intent of providing physicians with additional information about patients’ clinical picture, and ultimately enhance health care efficiency and delivery, the E4 wristband used in the pilot study at the Royal Melbourne Hospital, has become the primary tool of a new platform for vital sign monitoring: Empatica Care.
This newly-released remote health monitoring platform will enable providers (but also researchers and community leaders) to monitor patients with acute and chronic conditions, or healthy individuals who may be at risk of infection from a single dashboard, leading to better medical outcomes for all.
If you are interested in adopting Empatica Care for the remote health monitoring of your patients, research subjects, workforce, or local community, you can get in touch with our team here or send any questions directly to care@empatica.com. You can also visit Empatica.com/care to learn more.
CREDIT:
The scientific paper “Monitoring skin temperature at the wrist in hospitalised patients may assist in the detection of infection” was authored by Stephen G. Holt, Jennifer H. Yo, Connie Karschimkus, Frank Volpato, Steve Christov, Edward R. Smith, Tim D. Hewitson, Leon J. Worth, and Paul Champion De Crespigny.



