Using the E4 to assess sleep in caregivers of people with dementia

This article has been guest-authored by Reza Sadeghi, Ph.D. candidate of Computer Science and Dr. Tanvi Banerjee, Assistant Professor of Computer Science and Engineering at Wright State University, Dayton, OH USA.
Sleep forms roughly a third of our lives and affects our health and daily routines.
We all have experienced a lack of sleep, at some point, perhaps caused by stress in our personal lives, financial challenges, or even worrying about our loved ones. Lack of sleep can make us feel sleepy and tired the next day and can even result in a poor quality of work, or other responsibilities.
Caregivers of people with dementia (CPWD) are susceptible to poor sleep quality or inadequate sleep not just over one night but over extended periods of time, causing poor functioning during the day time, affecting their role as caregivers. The high stress of CPWD in providing care to their loved ones can reduce the chances of caregivers having uninterrupted sleep at night, especially due to the unpredictable dementia-related behaviors of their loved ones. As we can see, this can cause a vicious cycle that can lead to a state of physical, emotional, and mental exhaustion called caregiver burnout.
Most sleep assessment tools are not built for long-term monitoring. For example, polysomnography is a clinically established technique for measuring physiological signals during sleep (currently the gold standard for sleep measurement); however, it is expensive and is normally conducted in clinical centers. Using video cameras can be a solution for monitoring sleep in the home environment, but there are privacy concerns about their usage, especially since they have to be placed in the bedrooms of the participants. Another technique to measure sleep, actigraphy, can inexpensively and easily track the movements of subjects in bed better than pillow/bed sensors; however, these devices cannot report trends in other physiological signals, such as heart rate that can play an important role in sleep quality.
Wearable devices offer to monitor multiple physiological signals and can be proper tools in monitoring the sleep quality of the vulnerable groups.
The ease-of-use, cost-effectiveness, unobtrusiveness, and portability of wearable devices represent important advantages in monitoring the sleep of people, such as caregivers, in their homes.
As a researcher, we had access to and experimented with several wearable devices, both wrist-worn as well as others, such as smart vests. What drew us to the E4 wristband was the fact that it was non-invasive: from a user perspective it was just like a watch or a smart watch for the more technologically savvy. The other and the perhaps more crucial reason was that, unlike some of the other wrist-worn devices, the E4 provided raw sensor data, specifically photoplethysmogram (PPG), electrodermal activity (EDA), temperature, and accelerometer data.
The reliability of the E4 enabled us to easily schedule two-week experiments for monitoring the physiological signals of CPWD.
Predicting sleep quality
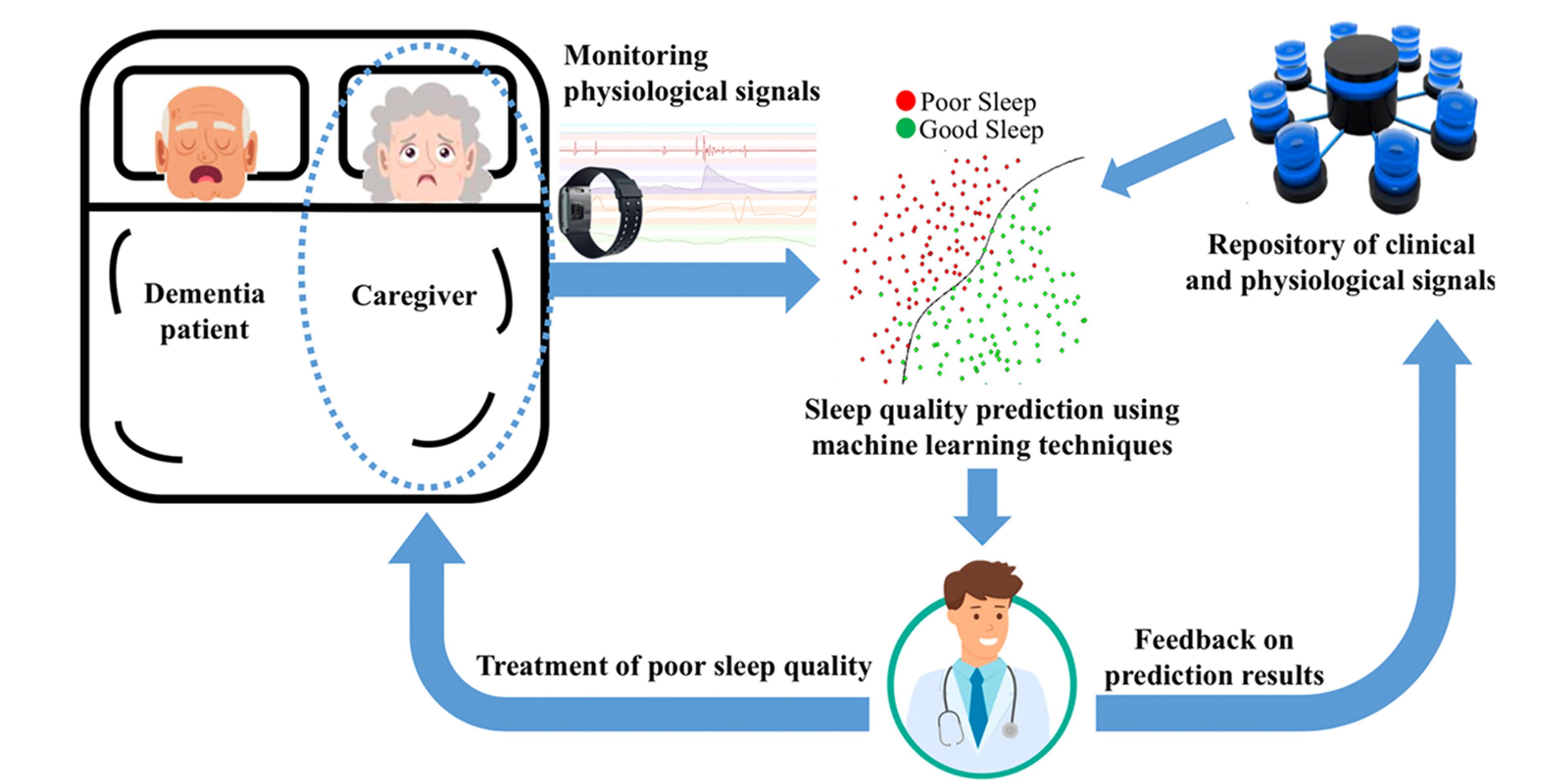
To aid both the caregivers of persons with dementia and their primary physicians, we designed a clinical decision support system - as shown in Figure 1.
We monitored the physiological signals of CPWD during their sleep using E4 wristbands. The collection of these physiological signals and the clinical history of CPWD formed our repository that was used to train machine learning techniques. Following this, we identified the sleep quality of new caregivers using trained machine learning techniques to be presented to their physicians. These results can aid physicians to provide the required intervention or social support resources to help alleviate the burden for caregivers. The feedback of physicians regarding the prediction outcomes is added to the repository of clinical and physiological signals to improve further predictions.
Although our participants were aged 65 and above, they easily learned how to use the device. Also, the secure cloud platform of Empatica allowed us to view and manage the recorded signals with ease. The users would wear the E4 devices fifteen minutes before bed-time, and remove them after they woke up. They would then charge the device which would be ready to use for the next night.
None of the participants mentioned any issues using the E4 devices, and we were able to gather high quality, high frequency raw physiological data for not just analyzing sleep quality, but also the different sleep stages that played a strong role in the overall mental state of the caregivers.
Because the battery life of the E4 is 36+ hours in memory mode, we didn’t have to worry about losing data if the caregivers forgot to charge the device once in a while. Having access to strong support staff at Empatica was also very helpful at the initial stages of our study when we were experimenting with the device.
In our published work in Computers in Biology and Medicine, we predicted the sleep quality of CPWD by tracking the physiological signals’ trends in the deep sleep stage, which is the sleep stage most associated with sleep quality and fatigue recovery. As shown in figure 2, this sleep prediction strategy enabled us to reuse the sleep investigations that have been conducted by polysomnography. Indeed, we followed trends in the deep sleep stage of recordable physiological signals by the E4 wristband that have been verified by polysomnography studies.
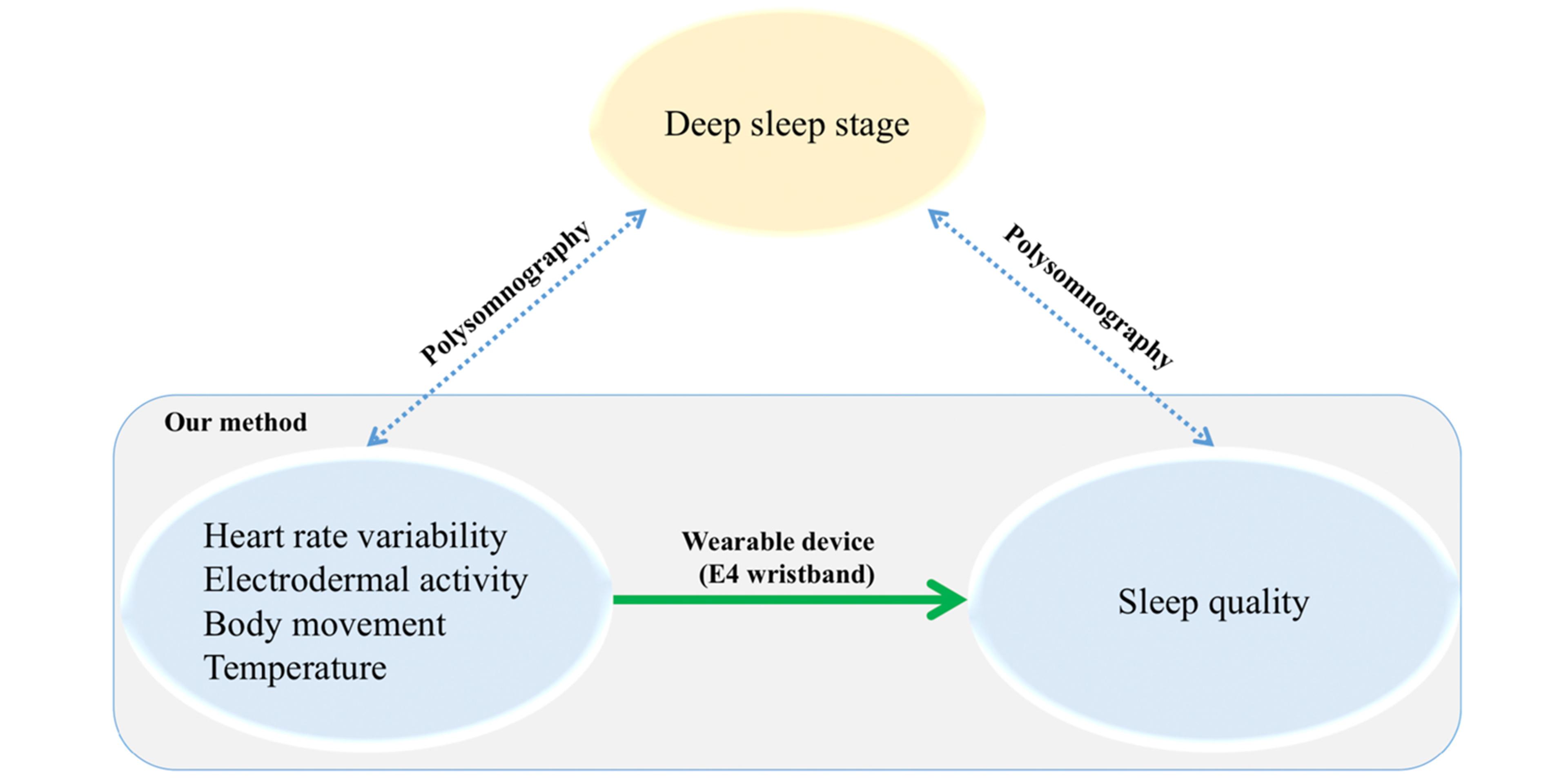
Since each signal has distinct characteristics in the deep sleep stage, we processed each signal differently intending to highlight the deep sleep portion of sleep. As detailed in our paper, we utilized a wide range of signal processing methods including Poincare plot to detect changes in correlation values between consecutive interbeat intervals, which are the time intervals between individual heartbeats. Following these signal processing methods, we extracted 20 (2 heart rate variability, 8 EDA, 7 body movement, and 3 temperature) features related to the deep sleep stage. We selected a subset of extracted features that maximize the accuracy of predicting sleep quality of CPWD using 10-fold recursive feature elimination. Next, we used three classifiers, naive Bayes, bagged tree, and random forest, to predict the sleep quality of CPWD. The source code of our method is publicly accessible: https://github.com/RezaSadeghiWSU/Sleep-quality-in-caregivers
Experimental results and clinical impacts
We examined 100 nights of sleep for eight CPWD to evaluate our proposed method. We asked the caregivers to wear the E4 wristband a quarter of an hour before their sleep time and take off the device after they wake up. Following this, they reported their quality of sleep through an Android tablet application. Although 82% of caregivers reported very good, good, or okay sleep quality, 65% of the caregivers described feeling tired after their sleep.
As mentioned earlier, the overwhelming caregiving responsibilities deprive CPWD of experiencing restful sleep. However, as they accustom themselves to the demanding caregiving tasks, the quality of their sleep is perceived as normal. As a result, we created two models based on physiological signals to predict both general sleep quality and feeling refreshed after sleep. In both models, the random forest classifier outperforms the other classifiers as it can handle nonlinearly separable data better than simpler classifiers, like naive Bayes.
In the sleep quality model, our proposed method automatically selected a subset of 18 signal-based features and reached an accuracy of 0.75. As our sleep quality model has a sensitivity of 0.75, it can correctly identify the five sleep quality categories (very good, good, okay, fairly bad, and bad) with a probability of 75%. Decreasing skin temperature plays the most significant role in the created model. This finding is in congruence with the fact that nocturnal temperature dysregulation as an age-related sleep disturbance can contribute to sleep fragmentation.
The feeling refreshed model distinguished feeling refreshed and tiredness sleep records with an accuracy of 0.73 using 12 extracted features from physiological signals. The proposed method can detect records of tiredness in caregivers with a high specificity of 0.94. In this model, sleep efficiency is the most important feature that describes the ratio of the amount of time asleep to the amount of time in bed. The significance of sleep efficiency is another sign of poor sleep quality in CPWD, who suffer from less total sleep time and longer transition time from wakefulness to sleep.
This work is extendable in various directions. In addition to examining our current cross-sectional study on a larger cohort of CPWD, we intend to design a longitudinal study to assess the sleep quality of CPWD over time and the role it specifically plays in caregiving. We will enhance the performance of our current sleep assessment by embedding personal behaviors in the form of a personalized sleep evaluation system. Also, we plan to examine the sleep quality of other communities susceptible to poor sleep quality.
In other research studies, we have been using the E4 device for measuring stress through sleep as well as gameplay to better understand how the galvanic skin response sensor changes with performance. We plan on continuing to use the E4 in other studies as we try to learn more about the role of physiology in our everyday lives.
You can learn more about the E4 wristband by visiting Empatica.com or getting in touch with the team here.
About the Authors:
Reza Sadeghi recently successfully defended his Ph.D. dissertation in Computer Science entitled “Predicting Subjective Sleep Quality using Objective Measurements in Older Adults.” During his graduate studies, he investigated applied machine learning in the fields of healthcare, web mining, and learning analytics. Throughout his Ph.D., he was a graduate research assistant of Dr. Tanvi Banerjee in the Data Science for Healthcare Lab at Wright State University. He was also a research trainee at the division of Sleep and Circadian Disorders at Brigham and Women's Hospital, Harvard Medical School. He is an active member of the Institute of Electrical and Electronics Engineers (IEEE), IEEE Engineering in Medicine and Biology Society (EMBS), and the American Thoracic Society (ATS).
Dr. Tanvi Banerjee is an Assistant Professor in the Department of Computer Science and Engineering, with a secondary appointment at the Department of Geriatrics, Boonshoft School of Medicine at Wright State University. Her research interest lies in using technology to solve healthcare challenges specifically to manage chronic conditions in domains such as sickle cell disease and dementia. Using standard easy to use mobile technology, she employs machine learning and signal processing techniques to manage patient symptoms remotely as well as sustainably. Her current research within the geriatric population includes using fitness devices for stress assessment in caregivers of patients with dementia (featured in local media sources, Alzheimer’s Association, as well as in the Research Features special issue of Women in Science, 2018), as well as in measuring pain in patients with sickle cell disease.



